If you’re working in healthcare, you know that handling sensitive health information comes with a huge responsibility. It’s not just about adhering to HIPAA compliances and avoiding HIPAA penalties — it’s about protecting patient confidentiality and trust.
Use this guide that breaks HIPAA down into simple, actionable insights. From what it is to why the healthcare law matters, we’ll share everything you need to manage Protected Health Information (PHI) based on our experience.
So, let’s begin.
What is HIPAA?
The Health Insurance Portability and Accountability Act (HIPAA) is a U.S. federal law enacted in 1996. It ensures the protection of sensitive patient health information (PHI) against unauthorized access. HIPAA applies to health care providers, insurance companies, and any business that handles PHI.
HIPAA is more than a compliance checklist; it’s a framework to ensure data privacy. It sets standards for secure electronic data exchange and defines how patient data should be stored, shared, and accessed.
Here’s what it promises:
- Patient privacy. Ensures sensitive data remains confidential;
- Standardized electronic health record. Defines secure methods for data transmission;
- Accountability. Sets penalties for violations or breaches;
- More control. Gives a patient rights over health data.
What is Protected Health Information?
Protected Health Information (PHI) is any data or information that can identify an individual in the process of availing health plans, or paying for healthcare services.
So, what is PHI information exactly? It includes:
- Medical records;
- Insurance details;
- Test results;
- Demographic information like name, phone number, or address;
- Biometric information like fingerprints or genetic data.
Both electronic and physical data are covered under what is considered PHI.
Individually Identifiable Health Information
Individually Identifiable Health Information is a subset of PHI that directly ties data to a specific person.
It includes unique identifiers like names, Social Security numbers, and medical record numbers. This data, when combined with health details, is considered PHI under HIPAA.
Core Components of HIPAA
The Health Insurance Portability and Accountability Act (HIPAA) is built on four essential pillars designed to protect patients’ sensitive health information.
These pillars or rules outline the framework an organization needs to implement to comply with HIPAA rules. Let’s look at all these important guidelines, including privacy and security rules.
HIPAA Privacy Rule
The HIPAA Privacy Rule outlines the standards to protect individuals’ medical records and personal health information (PHI). Issued by the U.S. Department of Health and Human Services (HHS), this rule limits the use and disclosure of PHI, ensuring only authorized entities access it.
Here’s what this rule states:
- Patients have the right to access their PHI upon request;
- They have the right to receive information on how their data is used;
- Covered entities (healthcare organizations and associates) must provide a clear account of PHI disclosures;
- Business associates must adhere to specific safeguards under formal agreements.
This rule ensures that even when PHI flows securely through multiple hands — health maintenance organizations, healthcare clearinghouses, insurance companies, and the health care system, patient information is always protected.
Health Insurance Portability
An important aspect of HIPAA is health insurance portability while protecting Protected Health Information (PHI).
Privacy Rule ensures patients can transfer their medical records, and health insurance records between providers without compromising privacy. This guarantees individuals continued health insurance coverage while setting clear guidelines to prevent unauthorized access to their medical history.
Health and Human Services
The Department of Health and Human Services (HHS) oversees the implementation and enforcement of the Privacy Rule, holding healthcare organizations accountable for protecting sensitive patient data.
HHS is responsible for maintaining a balanced framework where health information flows efficiently for care while respecting individual rights.
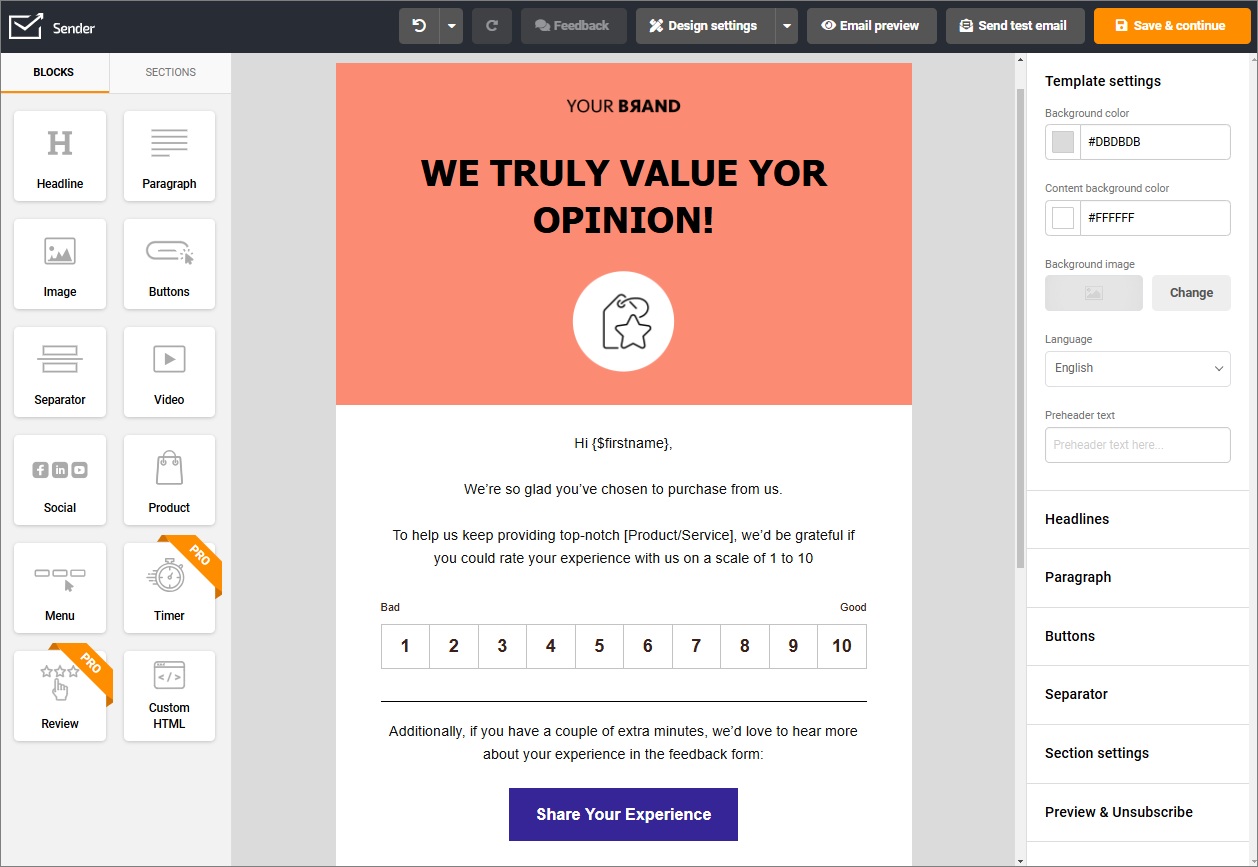
Send HIPPA-compliant emails with Sender. It’s safe, easy to use, and trusted by more than 180,000 successful businesses worldwide.
HIPAA Security Rule
The Security Rule helps organizations secure data by mitigating potential threats to patient data because of human, technical and environmental risks.
The rule sets a standardized security management process for the protection of electronic Protected Health Information (ePHI). It also outlines different risk management practices and safeguards to maintain health information privacy.
To comply with the Security Rule, organizations must implement three types of safeguards:
- Administrative. Requiring routine risk assessments and employee training to minimize human errors;
- Physical. To secure data storage locations, such as locked server rooms and controlled access areas, and;
- Technical. Setting encryption standards, securing data transmission protocols, and access controls to prevent unauthorized access.
Find more information about it here: HIPAA Secure Email: How to Send and Ensure Compliance
Electronic Protected Health Information
Electronic Protected Health Information (ePHI) covers all digital formats of patient data. It includes records like medical histories, prescriptions, and lab results in the electronic form.
The Security Rule protects patient information by outlining strict standards to ensure that ePHI remains confidential and accessible only to authorized personnel. Organizations must implement measures such as encryption, access controls, and regular risk assessments to protect ePHI against breaches and cyber threats.
HIPAA Breach Notification Rule
The Breach Notification Rule is designed to ensure transparency when patient data is compromised. It mandates that covered entities notify affected individuals, the Department of Health and Human Services (HHS), and in some cases, the media, following a breach of unsecured PHI.
This rule prioritizes patient safety and holds organizations accountable for their medical data security standards. Also, it protects individuals from fraud and builds trust through transparency.
Here are the general guidelines for complying with the breach notification rule:
- Breaches affecting over 500 individuals must be reported to HHS and publicized within 60 days;
- Smaller breaches must be reported by the end of the calendar year;
- Notifications to affected individuals must include details about the breach, the information compromised, and steps to mitigate risks.
For example, if a healthcare provider discovers unauthorized access to patient records due to a phishing attack, they must inform patients and provide resources to protect their identities, such as credit monitoring services.
HIPAA Enforcement Rule
The HIPAA Enforcement Rule ensures the accountability of covered entities towards patient data protection.
The rule covers how the Department of Health and Human Services (HHS) investigates, addresses violations of the Privacy, Security, and Breach Notification Rules, and imposes penalties for non-compliance.
Here’s what this rule outlines:
- Establishes procedures for resolving HIPAA violations;
- Imposes civil penalties based on the severity of non-compliance;
- Encourages organizations to proactively maintain compliance to avoid legal consequences.
In case of a violation, the rule kicks the enforcement process when a complaint is filed or a data breach is reported. It begins with an evaluation by the Office for Civil Rights (OCR). The OCR investigates whether the covered entity or business associate violated HIPAA regulations.
If violations are confirmed, the OCR works with the entity to resolve the issue through corrective actions. In severe cases, civil penalties are imposed, ranging from $100 to $50,000 per violation, depending on the degree of negligence.
FAQs about HIPAA
What is the primary purpose of HIPAA?
HIPAA ensures the privacy, security, and confidentiality of Protected Health Information (PHI). Its main goal is to protect sensitive health data, establish standards for secure information handling, and promise patients’ privacy.
What does HIPAA define as protected information?
Protected Health Information (PHI) under HIPAA includes any identifiable data about a patient’s identity as well as past, present, or future health. This includes names, addresses, medical records, Social Security numbers, and any biometric data, either in electronic, or paper, form.
What does it mean to comply with HIPAA regulations?
HIPAA compliance involves taking steps to protect PHI, ensuring privacy and security measures, and adhering to the reporting requirements. Covered entities and their business associates must follow rules like the Privacy Rule, Security Rule, and Breach Notification Rule.
Does HIPAA apply only to the United States?
Yes, HIPAA is a U.S. regulation governing healthcare organizations, insurers, and their associates handling PHI. However, its principles of data privacy and security influence global standards, and international entities working with US-based organizations must also adhere to HIPAA.
Is there a version of HIPAA in the European Union?
The European Union doesn’t have a direct equivalent to HIPAA. However, the General Data Protection Regulation (GDPR) provides appropriate data privacy protections, including health data. Unlike HIPAA, GDPR applies broadly across all industries, focusing on data privacy and user consent.
How does HIPAA compare to GDPR?
HIPAA focuses specifically on healthcare-related PHI within the U.S., while GDPR covers all personal data across various sectors in the EU. GDPR has broader applications, stricter consent rules, and applies globally to entities handling EU residents’ data. Both aim to protect sensitive information but differ in scope and enforcement policies.
Here are more related articles: