Protecting patient information isn’t just about laws—it’s about trust. Think about it: would you share personal details with someone who can’t keep them safe? Never!
If you’re in healthcare, you’ve probably heard the horror stories of hefty fines and shattered reputations from HIPAA violations. But here’s the good news: compliance doesn’t have to be a headache. In fact, when done right, it’s a win-win—patients feel safe, and your organization runs smoother.
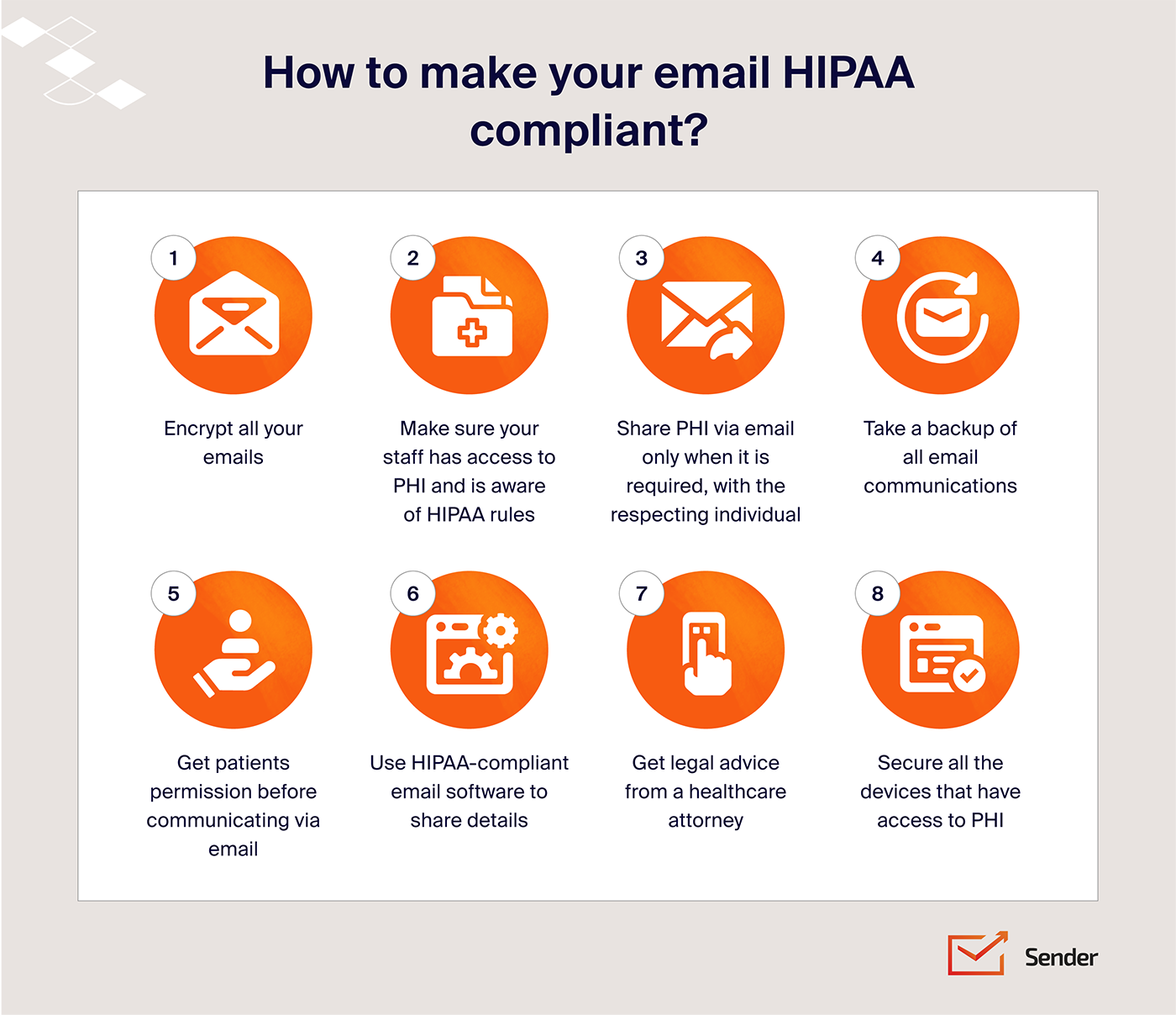
To make it easier, we’ve created a simple checklist to help you meet HIPAA policies and procedures for securing patient data. Let’s dive in!
What is HIPAA Compliance?
HIPAA compliance protects sensitive patient health information (PHI). Enacted in 1996, the Health Insurance Portability and Accountability Act sets rules to ensure PHI stays private, secure, and accessible only to the right people.
For HIPAA-covered entities like healthcare organizations, insurers, and their partners, HIPAA isn’t just a rulebook—it’s a trust-builder. From encryption to access controls, its privacy rules recommend the steps needed to keep PHI safe during storage, electronic communications, and handling.
Following HIPAA regulations shows more than just legal know-how — it demonstrates respect for patient privacy and a commitment to data security. It’s not just about avoiding fines; it’s about earning and keeping trust.
Why is it Important to Stay HIPAA Compliant?
If your organization handles Protected Health Information (PHI), HIPAA compliance isn’t optional—it’s mandatory.
Here’s what happens when you don’t comply:
- Massive fines: HIPAA violations can cost $100 to $50,000 each, with total penalties running into millions. Repeat offenses? That might even slap criminal charges;
- Reputation damage: A data breach shakes patient trust, making it harder to retain clients or partners;
- Operational chaos: Non-compliance invites audits, legal troubles, and expensive overhauls that disrupt routine business.
Staying compliant isn’t just about avoiding trouble. It shows your commitment to protecting patient privacy—building trust, and strengthening relationships with patients, clients, and partners.
Need to send HIPAA-compliant emails without the hassle? Sender makes it easy to stay secure and connect with your patients through emails.
9-Step HIPAA Compliance Checklist
HIPAA compliance requires more than just planning. It’s an ongoing commitment to protecting Protected Health Information (PHI). So, you need a checklist to manage your HIPAA compliance journey.
HIPAA Compliance Requirements Checklist
| Steps | Ask yourself |
| Assign Responsibility | Have you appointed a HIPAA compliance officer and created a cross-functional team? |
| Conduct a Risk Assessment | Have you identified risks, outlined vulnerabilities, and prioritized actionable solutions? |
| Develop Policies and Procedures | Have you drafted, updated, and trained staff on policies for handling PHI? |
| Implement Security Measures | Have you applied technical, physical, and administrative safeguards for PHI? |
| Establish Business Associate Agreements (BAAs) | Have you identified vendors handling PHI and established BAAs with clear breach protocols? |
| Implement Patient Rights Procedures | Have you provided patients with tools for accessing and controlling their PHI? |
| Set up a Breach Notification Rule | Have you set up a process to notify affected parties of breaches within 60 days and documented responses? |
| Monitor Compliance and Maintain Records | Are you regularly auditing practices, maintaining detailed logs, and using compliance software? |
| Train Your Workforce | Have you organized mandatory HIPAA compliance training with real-world scenarios? |
Let’s look at the actionable steps from the ultimate HIPAA compliance checklist for meeting HIPAA requirements as an organization.
1. Assign Responsibility
HIPAA compliance starts with accountability.
Appointing a compliance security officer ensures there’s someone dedicated to understanding and implementing HIPAA standards. This person will oversee policies, training, and audits, ensuring the team is up to date with regulations.
Here’s how to get started:
- Designate a HIPAA compliance officer to lead efforts;
- Create a cross-functional team to address specific compliance needs;
- Schedule regular updates to stay informed about regulatory changes.
2. Conduct a Risk Assessment
A thorough risk assessment is your first line of defense against vulnerabilities in your systems and processes.
By understanding where risks lie, you can take proactive measures to prevent breaches of PHI. This is not a one-time activity—it should be revisited regularly as new risks emerge.
Here’s how to get started:
- Identify all entry points to sensitive data, from physical records to digital systems;
- Clearly outline potential vulnerabilities and rate their severity;
- Focus on high-priority risks with detailed, actionable solutions.
3. Develop Policies and Procedures
Strong policies and procedures are the foundation of HIPAA compliance. They guide your team about securely handling Protected Health Information (PHI), covering everything from who can access it to how breaches should be managed.
Key steps to strengthen your policies and procedures:
- Draft comprehensive policies that cover PHI access, storage, and sharing to ensure consistency;
- Define breach protocols, including detailed steps for email security incident reporting and management;
- Update policies annually or whenever there are major operational or regulatory changes.
Remember, clarity is the key. Conduct regular training sessions about key practices and address any gaps in understanding.
4. Implement Security Measures
HIPAA mandates a combination of technical steps, physical security measures, and administrative safeguards for the confidentiality, integrity, and availability of patient data.
Here are the basic measures to protect sensitive information from unauthorized access, theft, or breaches:
- Use email encryption protocols like TLS for secure communication;
- Restrict facility access with ID-based security controls and entry systems;
- Train staff on handling PHI and documenting access logs.
Let’s look at each aspect one by one.
HIPAA Security Rule Checklist
| Requirement | Ask yourself |
| Technical Safeguards | Have you encrypted ePHI during storage and transmission, implemented access controls, and set up firewalls and intrusion detection? |
| Physical Safeguards | Have you restricted physical access to facilities, secured workstations, and ensured proper disposal of outdated records? |
| Administrative Safeguards | Have you created and implemented policies for PHI handling, conducted regular risk assessments, and trained employees on HIPAA standards? |
Technical Safeguards
With increasing cyber threats, robust technical measures are non-negotiable for compliance. Technical safeguards ensure the digital security of PHI.
These controls focus on protecting electronic protected health information (ePHI) during storage on a computer and transmission via technology.
Key actions for implementing technical safeguards:
- Encrypt emails and data during transmission and at rest using TLS protocols;
- Set up firewalls and intrusion detection systems to monitor network security;
- Implement access controls such as unique user IDs and two-factor authentication to restrict PHI access to authorized personnel;
- Regularly update software and systems to address vulnerabilities.
| Task | Ask Yourself |
| Create an Encryption Policy | Have you defined how ePHI is encrypted during transmission (e.g., TLS 1.2/1.3) and at rest? Have you specified encryption standards, approved tools, and key management procedures? |
| Document Access Control Policy | Are procedures in place for assigning unique user IDs to every individual accessing ePHI? Is two-factor authentication (2FA) enforced for added security?Are credential updates scheduled periodically to prevent unauthorized access? |
| Think of a Monitoring and Audit Policy | Have you documented how logging tools are used to track ePHI access? Are measures in place to detect and respond to unauthorized access activities? |
| Tools Required | |
| Encryption Tools | BitLocker, OpenSSL, or Sophos for encrypting files and emails. |
| Firewall & Intrusion Detection | Palo Alto Networks or Snort to monitor traffic and prevent unauthorized access. |
| Audit Logging Software | SolarWinds or Splunk to log and analyze access to PHI. |
Physical Safeguards
Physical safeguards secure the physical spaces and equipment used to store and access PHI. These measures minimize the chances of unauthorized access or accidental loss due to external factors.
Essential physical safeguards include:
- Restricting access to office facilities with PHI storage using ID-based entry systems;
- Securing workstations, filing cabinets, and servers with locks or biometric access;
- Implementing environmental controls such as fire suppression systems and temperature regulation;
- Ensuring proper disposal of outdated records and decommissioned devices containing PHI.
| Tasks | Ask Yourself |
| Create Facility Access Policy | Have you defined procedures for controlling physical access to areas containing ePHI?Do you utilize badge-based systems, biometric scans, or similar technologies for access control? |
| Set Up Workstation Security Policy | Are workstation locations and usage rules clearly specified for devices accessing PHI?Are automatic locking mechanisms enforced for unattended workstations? |
| Draft a Disposal Policy | Are secure disposal practices in place for outdated paper files and decommissioned devices?Is staff trained on proper disposal methods to ensure compliance? |
| Useful Actionable Tips | Use color-coded badge access for staff, contractors, and visitors.Create a secure room with zones marked as “PHI Access Allowed” and “PHI Access Prohibited.”Recommend webcam covers for workstations used remotely to protect privacy during telehealth sessions. |
| Tools Required | |
| Access Control Systems | HID Global or Kisi for badge or biometric-based entry |
| Secure Storage | Fireproof file cabinets or server racks with lockable features |
| Shredding Equipment | Fellowes Powershred or shredding services like Shred-it for secure document disposal. |
Administrative Safeguards
Define clear procedures for handling PHI and train staff accordingly. Regular audits can identify security gaps and opportunities for improvement.
Steps to implement administrative safeguards:
- Develop and document policies for accessing, storing, and transmitting PHI;
- Conduct regular risk assessments to identify and address vulnerabilities;
- Provide HIPAA training to employees, contractors, and business associates;
- Maintain detailed records of access logs and system usage.
| Tasks | Ask Yourself |
| Create a Risk Assessment Policy | Have you defined steps to conduct periodic risk analyses to identify vulnerabilities in ePHI handling? Are the findings documented and used to improve safeguards? |
| Think of a Training Policy | Is mandatory HIPAA training scheduled for all staff handling PHI? Are refresher sessions conducted regularly to keep staff updated? |
| Plan an Incident Reporting Policy | Are protocols in place for identifying, reporting, and addressing breaches? Do the protocols include clear timelines and escalation processes? |
| Tools Required | |
| Risk Assessment Tools | Compliancy Group or HIPAA Secure Now! for comprehensive evaluations. |
| Training Platforms | Healthstream or MedTrainer for HIPAA-specific employee training. |
| Incident Management: | ServiceNow or Freshservice for tracking and resolving compliance incidents. |
5. Establish Business Associate Agreements (BAAs)
Collaborating with third-party vendors handling PHI requires signing a Business Associate Agreement (BAA). This ensures they follow HIPAA standards and take responsibility for any breaches or unauthorized disclosures.
Regularly review agreements to ensure they align with current regulations and address any new risks. Consider including clauses about subcontractor compliance if your associates rely on third-party services.
Here’s how you can get started with BAAs:
- Identify all vendors managing PHI and establish BAAs;
- Define clear breach reporting procedures in agreements;
- Regularly audit business associates for HIPAA compliance.
6. Implement Patient Rights Procedures
Patients have the right to access and control their medical information under HIPAA.
Your organization must provide clear directions for patients to request records, correct inconsistencies, or obtain details about their PHI usage. Responding in time to patient requests helps avoid potential legal issues and builds trust.
Here’s what you should do to implement these procedures:
- Create a portal for PHI access and amendment requests;
- Provide clear timelines for responding to patient inquiries;
- Document every patient interaction for accountability.
7. Set Up Breach Notification Protocols
A proactive breach notification plan is critical. HIPAA requires you to inform affected individuals and regulatory authorities within specific timeframes if PHI is compromised.
Preparation is key. Simulate breach scenarios to refine your response plan and ensure your team knows exactly what to do in an emergency.
Here’s your action plan to set up these protocols:
- Notify affected parties within 60 days of discovering a breach;
- Keep detailed records of breach investigations and responses;
- Conduct regular training on breach identification and reporting.
8. Monitor Compliance and Maintain Records
HIPAA compliance is an ongoing process. Regular monitoring ensures your organization stays ahead of risks and passes necessary due diligence during audits.
Regular monitoring not only simplifies audits but also helps identify areas for improvement.
Here’s what you can do:
- Audit PHI management practices quarterly or semi-annually;
- Maintain logs of access, training sessions, and policy updates;
- Use compliance software for streamlined tracking and reporting.
HIPAA Audit Checklist
| Audit Step | Ask Yourself |
| Review Risk Assessment Reports | Have you ensured that risk assessments are comprehensive and regularly updated? |
| Verify Policies and Procedures | Do your policies address PHI access, storage, and breach protocols effectively? |
| Examine Security Measures | Are technical, physical, and administrative safeguards in place and functioning? |
| Check Business Associate Agreements (BAAs) | Are BAAs signed and updated for all vendors handling PHI? |
| Evaluate Breach Notification Procedures | Have you checked response timelines and documentation requirements for breach handling? |
| Inspect Workforce Training Records | Are training sessions documented, and is the workforce compliant with HIPAA standards? |
| Audit PHI Access Logs | Have you reviewed access logs for irregularities or unauthorized access? |
9. Train Your Workforce
Your workforce is the front-line force for HIPAA compliance. Regular training ensures employees understand their responsibilities and how to avoid common pitfalls when handling PHI.
Here’s what you should do to create engaging training programs as an employer:
- Organize mandatory HIPAA training during onboarding;
- Include real-world scenarios in training sessions;
- Offer refresher courses whenever policies or staff roles change.
HIPAA Compliance Checklist FAQs
What is the minimum necessary requirement in HIPAA compliance?
The “minimum necessary requirement” under HIPAA says that only the least amount of Protected Health Information (PHI) required for a specific task should be accessed, used, or disclosed. This ensures patient data is shared on a strict need-to-know basis. For example, a billing staff member would access payment details but not the full medical record.
Is full-disk encryption mandatory under HIPAA?
No, full-disk encryption isn’t mandatory, but it’s highly recommended. HIPAA requires ePHI to be secure during storage and transmission, and encryption is a key safeguard. Full-disk encryption protects all device data, reducing the risk of unauthorized access and showing commitment to HIPAA standards.
What are the requirements for a HIPAA-compliant backup system?
A HIPAA-compliant backup system must securely store encrypted ePHI and ensure data integrity and availability. Backups should be performed regularly and stored offsite to mitigate risks from local disasters. The system must also provide access controls to limit unauthorized use. Additionally, organizations should test backup restoration periodically to ensure reliability.
HIPAA regulations is a vast topic, here’s some more valuable content: